"Everything you said would happen following the procedure, did. I wasn't surprised at anything...Thank you again for being so thorough and honest. You rock."
-Alexandra
Information on this page is for women who have decided to proceed with UFE.
Insurance pre-certification: To be certain that you will not have any problems with your insurance company after the procedure, it is best to get their OK up front. This go-ahead is called pre-certification or pre-authorization. We will help you obtain this "all clear" from your insurance company, if they require it. It all starts with a call to the IRC at 210.616.7780.
Procedure day details: A nurse from the radiology department at Methodist will try to call you during the afternoon before your procedure (or on Friday if you procedure is scheduled for Monday) to go over these instructions and answer questions. Try to answer the phone when they call as it is a good idea to speak with the nurse. Generally you will come to the hospital between 6:30 and 7:00 in the morning; you cannot eat anything for 6 hours before UFE so it is best to get it done after a night of fasting. If you usually take medications in the morning, like high blood pressure medicine, go ahead and take them but with just small sips of water. Leave valuables at home to reduce risk of losing something at the hospital. You will need to have someone take you home after your procedure (or the next morning if you stay the night). It is hospital policy that you may not take an Uber/Lyft/Cab; you have to leave with a human you know.
You either come directly to the Radiology Department on sublevel 2 of Methodist Hospital or you will be asked to go to the laboratory. Do not go to the admissions desk on the first floor.
You will get registered at the Radiology Front Desk and meet our nurses in our Holding Area. You will change into a hospital gown; it is a good idea to leave your valuables at home. One of our nurses will start an IV in your arm. When your procedure is over you will need to stay at bedrest for at least 2 hours, sometimes 4 hours. If you have to urinate during that time you will have to use a bedpan. If you would rather not have to struggle with a bedpan we can place a tube into your bladder (Foley catheter), and this is a good time to get that done if you think you need it. I will go over things with you a final time and we will ask you to give your consent for the procedure and sign the hospital consent forms. We will give you some medications through your IV that get you ready for the procedure, including an antibiotic (usually cefazolin), a medicine the reduces nausea (Zofran), and another that stops pain and inflammation (Toradol and Decadron). You are transferred from the Holding Area to the procedure room. If you bring friends or family with you this is when you say goodbye, you will see them again as soon as your procedure is over.
Insurance pre-certification: To be certain that you will not have any problems with your insurance company after the procedure, it is best to get their OK up front. This go-ahead is called pre-certification or pre-authorization. We will help you obtain this "all clear" from your insurance company, if they require it. It all starts with a call to the IRC at 210.616.7780.
Procedure day details: A nurse from the radiology department at Methodist will try to call you during the afternoon before your procedure (or on Friday if you procedure is scheduled for Monday) to go over these instructions and answer questions. Try to answer the phone when they call as it is a good idea to speak with the nurse. Generally you will come to the hospital between 6:30 and 7:00 in the morning; you cannot eat anything for 6 hours before UFE so it is best to get it done after a night of fasting. If you usually take medications in the morning, like high blood pressure medicine, go ahead and take them but with just small sips of water. Leave valuables at home to reduce risk of losing something at the hospital. You will need to have someone take you home after your procedure (or the next morning if you stay the night). It is hospital policy that you may not take an Uber/Lyft/Cab; you have to leave with a human you know.
You either come directly to the Radiology Department on sublevel 2 of Methodist Hospital or you will be asked to go to the laboratory. Do not go to the admissions desk on the first floor.
You will get registered at the Radiology Front Desk and meet our nurses in our Holding Area. You will change into a hospital gown; it is a good idea to leave your valuables at home. One of our nurses will start an IV in your arm. When your procedure is over you will need to stay at bedrest for at least 2 hours, sometimes 4 hours. If you have to urinate during that time you will have to use a bedpan. If you would rather not have to struggle with a bedpan we can place a tube into your bladder (Foley catheter), and this is a good time to get that done if you think you need it. I will go over things with you a final time and we will ask you to give your consent for the procedure and sign the hospital consent forms. We will give you some medications through your IV that get you ready for the procedure, including an antibiotic (usually cefazolin), a medicine the reduces nausea (Zofran), and another that stops pain and inflammation (Toradol and Decadron). You are transferred from the Holding Area to the procedure room. If you bring friends or family with you this is when you say goodbye, you will see them again as soon as your procedure is over.
The Procedure Room
This procedure room, an Angiography room, contains a special x-ray machine that allows me to use real-time x-ray (called fluoroscopy). That's it behind us in the photo.
Here you will meet our technologists. They are specially trained to assist me during the procedure. You will be asked to slide over from you stretcher onto the angio table. We then do the final preparation by cleansing the skin at your groins with an antimicrobial soap. This soap is great for killing bugs on the skin but works best if there is no hair. So if needed we will clip away any hair at the site we are cleaning. A large drape, like a bed sheet, is placed over you to provide a barrier to infection. So the only part of you that is exposed below your chin are two small circles, one at each groin, and the area just below your naval.
We have a sound system in the angiography suite. Music can help you take your mind off of all the technical things happening in the room, and we are happy to listen to whatever type of music you wish; pick and artist or song and we will create a Pandora station for you. Or you can take your chances and listen to our music! You are going to be in this room for about 90 minutes.
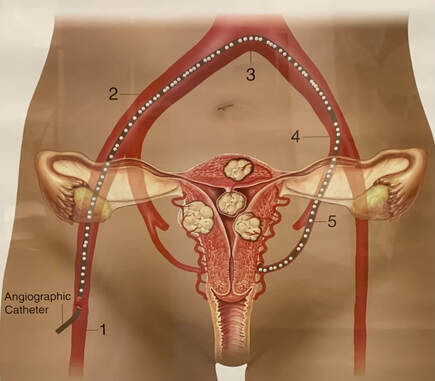
Our nurse will give you some medicines through your IV that will help you be relaxed and stop pain (usually Versed and Fentanyl). I put some medicine into the skin, usually the right side, where the catheter will be passed into the artery. This is a local anesthetic (Xylocaine) that makes the area numb; the same medicine a dentist uses. I will make a tiny nick in the skin through which I puncture the artery and pass the catheter that I use for the embolization. I use ultrasound to guide this puncture so it is extremely accurate and done with a very tiny needle. Typically, you feel none of this manipulation. When I make the injections to see the arteries most women feel a warm sensation in the pelvis and at first it feels like you are urinating (you aren't, it just feels like it). The uterus has two main arteries, one from the right and one from the left. I can usually get to both uterine arteries from one side but rarely I need to come from both groins to get both arteries. When the catheter is safely within the uterine artery I will block off the artery by injecting small particles. These small particles are what stop the blood flow to the fibroids causing them to die and shrink. After I complete the embolization of the left artery I will give you a nerve block so that you do not feel pain when I embolize the right side. When the embolization is complete we remove the catheter from the artery and place a small device under the skin to help the artery not bleed. The device will be absorbed by your body after a week or so. We also hold pressure on the site for about 5 minutes.
Then we transfer you back to your stretcher and you go back to the holding area. Once our nurses have you situated they will allow your family/friends to see you. Since we have limited space we ask that patients have just one visitor at a time.
With the nerve block you should have only moderate pain that changes to a sensation of pressure in your pelvis after about 30 minutes. This is a temporary sensation that will be gone by evening or perhaps the following morning. As the block wears off, you might notice pain is getting worse in your pelvis, this does not mean anything is going wrong, it is just the block wearing off...you are already on the other side of what would have been very significant pain 8-12 hours after the procedure.
The discomfort you have in your pelvis will wax and wane over the next several days, but each day you will feel a little better than before. The post-embolization syndrome will cause you to feel tired and have a low-grade fever for a few days. We will prescribe that you take ibuprofen (the same medicine in Advil, but a higher dose) for one week to help keep the post-embolization syndrome in check as well as an antibiotic to prevent infection. We will also give you some prescriptions for pain medications that you can take if needed.
We ask that you come back to see us in three months.
Also, you can email me anytime. I tend to be more accessible by email than by phone since I am often in a procedure during the day and cannot come to the phone.
Our nurses will be in contact with you to see how you are doing in a day or so after your UFE, and possibly later as part of our long term follow-up.
Here you will meet our technologists. They are specially trained to assist me during the procedure. You will be asked to slide over from you stretcher onto the angio table. We then do the final preparation by cleansing the skin at your groins with an antimicrobial soap. This soap is great for killing bugs on the skin but works best if there is no hair. So if needed we will clip away any hair at the site we are cleaning. A large drape, like a bed sheet, is placed over you to provide a barrier to infection. So the only part of you that is exposed below your chin are two small circles, one at each groin, and the area just below your naval.
We have a sound system in the angiography suite. Music can help you take your mind off of all the technical things happening in the room, and we are happy to listen to whatever type of music you wish; pick and artist or song and we will create a Pandora station for you. Or you can take your chances and listen to our music! You are going to be in this room for about 90 minutes.
Our nurse will give you some medicines through your IV that will help you be relaxed and stop pain (usually Versed and Fentanyl). I put some medicine into the skin, usually the right side, where the catheter will be passed into the artery. This is a local anesthetic (Xylocaine) that makes the area numb; the same medicine a dentist uses. I will make a tiny nick in the skin through which I puncture the artery and pass the catheter that I use for the embolization. I use ultrasound to guide this puncture so it is extremely accurate and done with a very tiny needle. Typically, you feel none of this manipulation. When I make the injections to see the arteries most women feel a warm sensation in the pelvis and at first it feels like you are urinating (you aren't, it just feels like it). The uterus has two main arteries, one from the right and one from the left. I can usually get to both uterine arteries from one side but rarely I need to come from both groins to get both arteries. When the catheter is safely within the uterine artery I will block off the artery by injecting small particles. These small particles are what stop the blood flow to the fibroids causing them to die and shrink. After I complete the embolization of the left artery I will give you a nerve block so that you do not feel pain when I embolize the right side. When the embolization is complete we remove the catheter from the artery and place a small device under the skin to help the artery not bleed. The device will be absorbed by your body after a week or so. We also hold pressure on the site for about 5 minutes.
Then we transfer you back to your stretcher and you go back to the holding area. Once our nurses have you situated they will allow your family/friends to see you. Since we have limited space we ask that patients have just one visitor at a time.
With the nerve block you should have only moderate pain that changes to a sensation of pressure in your pelvis after about 30 minutes. This is a temporary sensation that will be gone by evening or perhaps the following morning. As the block wears off, you might notice pain is getting worse in your pelvis, this does not mean anything is going wrong, it is just the block wearing off...you are already on the other side of what would have been very significant pain 8-12 hours after the procedure.
The discomfort you have in your pelvis will wax and wane over the next several days, but each day you will feel a little better than before. The post-embolization syndrome will cause you to feel tired and have a low-grade fever for a few days. We will prescribe that you take ibuprofen (the same medicine in Advil, but a higher dose) for one week to help keep the post-embolization syndrome in check as well as an antibiotic to prevent infection. We will also give you some prescriptions for pain medications that you can take if needed.
We ask that you come back to see us in three months.
Also, you can email me anytime. I tend to be more accessible by email than by phone since I am often in a procedure during the day and cannot come to the phone.
Our nurses will be in contact with you to see how you are doing in a day or so after your UFE, and possibly later as part of our long term follow-up.